Advances in Animal and Veterinary Sciences
Research Article
Advances in Animal and Veterinary Sciences 2 (5): 270 – 276Effect of medical grade chitosan powder in full thickness skin wound healing in rat model
Kumar Sandeep, Swapan Kumar Maiti*, Kumar Naveen, Malik Mohammad Sams-uz-Zama, Ninu Ajantha Ravindran, Ashok Kumar Balwada, Dayamon David Mathew
- Division of Surgery, Indian Veterinary Research Institute, Izatnagar, 243122(UP), India
*Corresponding author: maiti_62@rediffmail.com; swapanivri@gmail.com
ARTICLE CITATION:
Sandeep K, Maiti SK, Naveen K, Sams-uz-Zama MM, Ninu AR, Balwada AK, Mathew DD (2014). Effect of medical grade chitosan powder in full thickness skin wound healing in rat model. Adv. Anim. Vet. Sci. 2 (5): 270-276.
Received: 2014–02–22, Revised: 2014–04–13, Accepted: 2014–04–14
The electronic version of this article is the complete one and can be found online at
(
http://dx.doi.org/10.14737/journal.aavs/2014/2.5.270.276
)
which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
ABSTRACT
The present study was conducted in 18 wistar rats of either sex divided into two equal groups (n = 9) to evaluate the healing potential of medical grade chitosan powder. One 20 X 20 mm2 full thickness skin wound was created on dorsal region of thorax of adult wistar rats. Topical application of paraffin gauze over the wound acted as control (Group - A). In second group (Group - B) of animals, wounds were treated with sterilized, medical grade chitosan powder. The wounds were evaluated based on clinical and macroscopical parameters. Gross observations and photographic evaluations were also done until the end of the study. Clinical observations, gross observation, exudation, granulation tissue, peripheral swelling and the contraction rate of the wounds were recorded on days 0, 3, 7, 14, 21 and 28 days post surgery at different intervals in both the groups. Early granulation tissue formation with reduced exudation and peripheral swelling was observed in treatment group-B and proved better than that of group - A. The percent of wound contraction was similar to those gross findings, however, in group - B, complete wound healing was observed on day 20 - 22, but in group-A (control), healing was completed by day 27 - 28.
INTRODUCTION
Skin wounds are physical injuries that result in an opening or breaking of the skin. Disruption of skin generally leads to increase fluid loss, infection, hypothermia, scarring and compromised immunity (Nalbandian et al., 1987; Wysocki, 1999). A wound may be defined as disruption of the cellular or anatomical continuity of the normal organ structure. Wound healing is an evolutionarily conserved skin, aims at barrier restoration. Wound repair is a complex process requiring coordination of cascade of cellular responses to injury including inflammation, epithelialization, proliferation, angiogenesis and remodeling. Healing involves migration, infiltration, proliferation, and differentiation of several cell types like keratinocytes, fibroblasts, endothelial cells, macrophages, and platelets which were culminate in an inflammatory response, the formation of new tissue and wound closure (Barrientos et al., 2008).
Chitosan is a 1, 4 - linked polymer of glucosamine (2 -amino – 2 – deoxy – D - glucose) and lesser amounts of N -acetylglucosamine. It is a derivative of chitin (poly – N -acetylglucosamine) which is the second most abundant biopolymer after cellulose. It is biocompatible, biodegradable, haemostatic, anti-infective and, more importantly, it accelerates wound healing (Ishihara et al., 2002). Chitosan is a biodegradable polymer and it accelerates wound healing (Conti et al., 2000). It has been reported that chitosan permits regeneration of tissue elements in skin wounds and has positive application effects on wound healing (Bartone, Adickes et al., 1988). Also, chitosan exhibits many advantages for topical application, including good flow properties, non-irritancy, some antibacterial effect and a potential for a suitable release rate from the dosage form (Bartone, Adickes et al., 1988). With this background, the present study was designed with the objective to evaluate healing potential of medical grade chitosan powder for full thickness skin wounds in wistar rats.
MATERIALS AND METHODS
Eighteen clinically healthy adult wistar rats of either sex were used in this study. All the animals were procured from Laboratory Animals Research (LAR) section of Indian Veterinary Research Institute, Izatnagar, Uttar Pradesh, India. Each animal was caged individually and provided free access to water and a standard diet all the animals were maintained under standard conditions. All the animals were acclimatized to approaching, handling and animal house conditions for a period of 10 - 15 days prior to the study. They were randomly divided into 2 groups, viz., Group A and B of 9 animals each.
Surgical procedure
The rats were anaesthetized using xylazine at a dose rate of 5 mg/kg and ketamine at a dose rate of 50 mg / kg administered intramuscularly (Gangwar et al., 2013). The animals were placed in sternal position on the operative table.
The animal was prepared aseptically (Figure: 1) by shaving the dorsal area starting from the caudal part of the blades of the shoulder on the dorsum to the caudal part of the last rib. The area was scrubbed and later was painted with povidone iodine (Gangwar et al., 2013). On the prepared area, a 20x20 mm2 full thickness skin defect was created aseptically (Figure: 2).
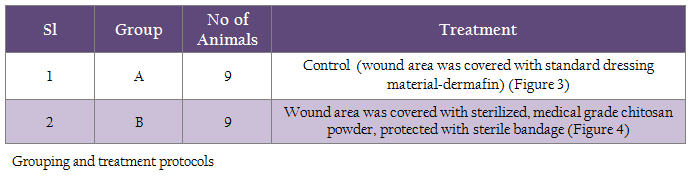
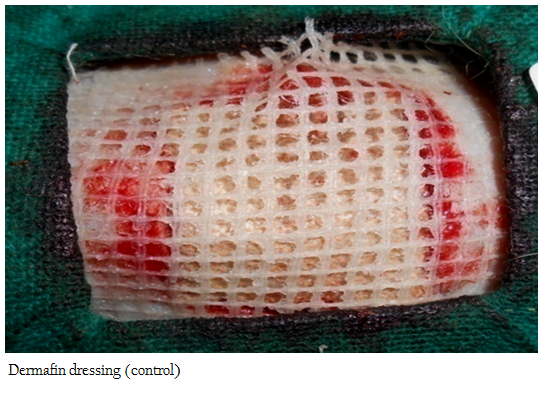
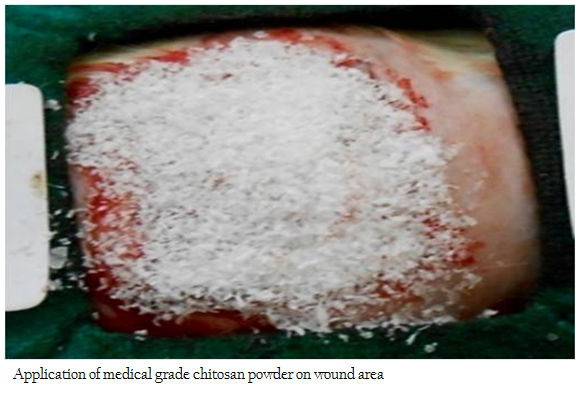
The animals in each group were treated as described in table - 1. The wounds were observed for 28 days or till complete healing of the wound. The efficacy of the wound healing was measured on the basis of following parameters.
Clinical observations
a) General behavioral changes: Feeding pattern and general behavioral changes in all the animals was observed daily during the observation period; b) Rectal temperature: Rectal temperature was recorded daily upto 7 postoperative days in all the animals; c) Warmth: The warmth of the adjoining area was measured using digital thermometer daily upto 7 postoperative days.
Gross observations
The wound site was examined grossly on days 0, 3, 7, 14, 21 and 28 or till completion of healing for the evaluation of following parameters:
a) Measurement of wound area: Wound area was measured at day 0, 3, 7, 14, 21 and 28 or till completion of healing.
b) Wound contracture: Wound contraction was measured on 0, 3, 7, 14, 21, and 28 postoperative day as a percentage reduction in wound area (Parameshwaraiah, Shivakumar et al., 1998). Progressive decrease in the wound area was monitored periodically by tracing the wound margins on a tracing paper and the area was assessed by using a graph paper. The total wound area of each tracing was subtracted from that of the initial tracing to determine the extent of contraction at each interval. The mean wound area and the mean percentage of wound contraction for each interval were calculated for each group (Bigbie et al., 1991; Bohling et al., 2004).
Total wound area on dayn
% conc. = (100 - ________________________ X 100) / Original wound area on day 0
Where n is: 0,3,7,14,21 and 28 day.
c) Exudation: The degree of exudation at the site of repair was graded on 1-4 scale as per standard method (Bigbie et al., 1991) = none (apparently dry wound); 2 = Mild exudates (wound is moist, no oozing on pressing the wound); 3 = Moderate exudates (wound is moist, slight oozing on pressing the wound); 4 = Extreme exudates (exudates is visible and pressure lead to extensive exudation).
d) Degree of Pain: The degree of pain was assessed by gently pressing the operation site and was graded on 1 - 4 scale as follows: 1 = No pain on extensive manipulation; 2 = Mild pain on extensive manipulation; 3 = Moderate pain on moderate manipulation; 4 = Severe pain on slight manipulation.
e) Degree of peripheral swelling: The degree of peripheral swelling in open wounds was evaluated and graded as; 1 = Nil; 2 = Moderate; 3 = Marked.
f) Evaluation of granulation tissue: Granulation tissue evaluation was graded on 1 - 4 scale as per standard method (Bigbie et al., 1991), 1 = Granulation tissue depressed below the skin edge; 2 = Granulation tissue proliferated to the level of skin edge; 3 = Granulation tissue elevated above skin edges; 4 = Granulation tissue elevated above skin edges, projecting over the border of epithelium.
g) Colour of granulation tissue: Colour of the wound depicts the status of healing and was scored as: 1 = Pale yellow; 2 = Pale red and 3 = Pink.
h) Time of appearance of granulation tissue: It was recorded as the first day when the granulation tissue was observed.
Colour Digital Image Processing
Digital colour photographs were taken on days 0, 3, 7, 14, 21 and 28 or till completion of healing with the help of digital camera. Analysis of shape, size, irregularity and colour of the lesion was determined.
Statistical Analysis
The data was analyzed by using the suitable Statistical Program for Social Sciences (SPSS) for windows (Snedecor and Cochran, 1989). The data were analyzed by using the Statistical Program for Social Sciences (SPSS) software version 16.0. One way ANOVA (Analysis of Variance) and Duncan’s multiple range test (DMRT) were used to compare the means at different time intervals among different groups. Student’s paired‘t’ test was used to compare the mean values at different time intervals with their base values in each group (Snedecor, Cochran et al., 1989). The subjective data generated from the scoring of various parameters were analyzed using Kruskal Wallis test.
Ethical Permission Necessary permission was undertaken from the Institute Animal Ethics Committee (IAEC), Indian Veterinary Research Institute, Izatnagar (UP), India to conduct this research wok on small laboratory animals.
RESULTS
Animals of both groups started taking feed and water partially within 24h of surgery. In all the animals feed and water intake became normal by 3rd postoperative day. The animals remained slightly dull for first 2 days after surgery. Almost all the animals of both groups assumed a hunched back posture while resting in their cages for 1 - 2 days after surgery. The animals of groups B started taking rest in dorsal recumbency from day 13. The animals of control group started to rest on its back after 18 days.
The mean rectal temperature increased significantly (P < 0.05) in all the animals of both groups up to day 3 postoperatively. The peak values were recorded on day 3 in both groups. Thereafter, gradual decrease in temperature was observed in both groups. The temperature reached within normal limits by day 7. On day 3, temperature was significantly increased within group A. On day 4, temperature was decreased significantly (P < 0.05) in group B as compared to group A.
The warmth of the wound was compared with the warmth of the adjacent tissue using electronic digital thermometer. In both the groups the temperature of the adjacent tissue was found higher than the temperature of the wound on day 3 and day 7 postoperatively. No significant difference (P > 0.05) in temperature was observed between the groups.
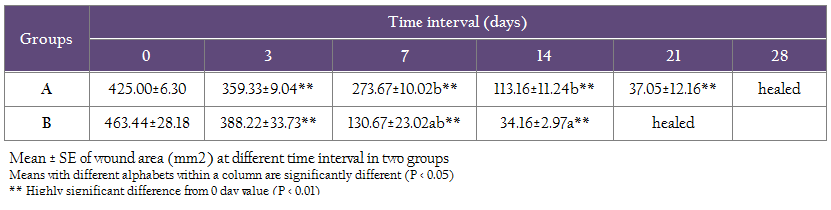
With the passage of time, a gradual decrease in wound area (mm2) was observed in both groups during the entire observation period. Mean ± SE of the total wound area (mm2) of the skin wounds at different time interval are presented in table- 2. On day 7 and 14, wound areas were significantly (P < 0.05) decreased in group B as compared to group A. Complete wound healing was recorded on day 27-28 in group A, whereas in group B, it was observed much earlier i.e. 20 - 22 postoperative day.
Original wound was created as 2 cm X 2 cm dimensions, however, almost all the wounds expanded to various extents and had an area greater than the 4cm2. Significant (P < 0.05) increase in percent of contraction was observed in both the groups during the observation period. On day 7 and 14, wound area was significantly (P < 0.05) contracted in group B as compared to group A. Mean ± SE of the total wound area contraction at different time interval are presented in table - 3.
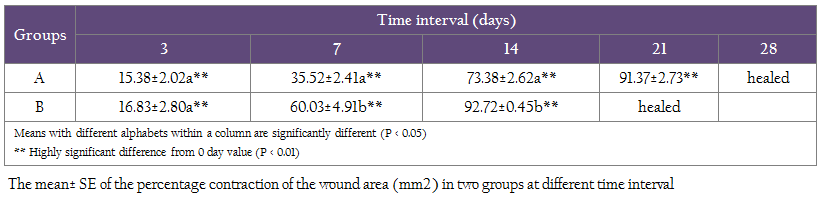
Table 3: The mean± SE of the percentage contraction of the wound area (mm2) in two groups at different time interval
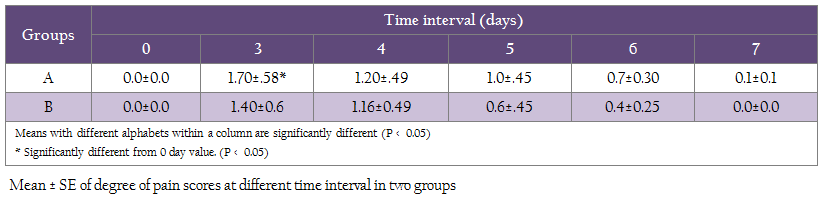
Moderate exudation at the site was observed upto day 3 - 5 in treated as well as control wounds. But in animals of group A showed a significantly higher (P < 0.001) values of exudation on day 3 and 6 respectively as compared to group B In both groups, moderate pain was observed on day 3 after operation. As the wound healing progressed, lesser intensity of pain was observed in both groups. Pain scores were decreased by day 3 onwards. On day 3, pain was significantly (P < 0.05) increase in group A where it was decreased in group B. The mean ± SE degree of pain at the operated site is presented in table- 4. Peripheral swelling of moderate value (score 2) was present in animals of both groups. This underwent reduction, recorded from day 3 onwards. In group, B, there was a drastic reduction in peripheral swelling was recorded on day 7. From day 3 and day 7, there were significantly differences within the groups in terms of swelling.
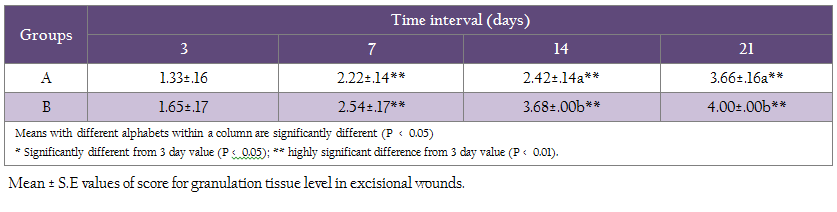
In group A, granulation tissue was not so discernible by day 3, however, some areas of granulation tissue formation was observed towards the periphery. Granulation tissue was formed below the skin edge between day 3 and day 7 and proliferated to the level of skin edges by day 7 post wound in group B significantly. Animals of group B showed significantly higher granulation tissue values (P < 0.05) on day 14 and day 21 as compared to group A (Table 5).
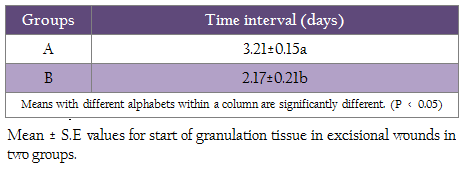
The time (day) of appearance of granulation tissues seen grossly was significantly (P< 0.05) less in group B than group A (table - 6). Creation of excisional wounds resulted in variable extent of bleeding and formation of clot. The clot was dried and formed a cover over the wounds, which rendered the evaluation of colour of granulation tissue difficult in some of the animals. The scab, which covered the underlying granulation tissue, was detached in majority of the wounds before 21st postoperative days. At this junction the classical ‘shinny, beefy, red’ to pink granulation tissue indicating healthy healing progress was evident.
The scar became paler with passage of time, which indicated stage of maturation. The maturation was much earlier in group B than group A. The colored digital photographs of wounds in animals of group A revealed that the wounds were covered with soft and fragile pinkish mass having mildly desiccated top surface on day 3. On day 7, the surface became desiccated and somewhat necrosed. By day14, thick granulation appears and size of wound decreases. By day 21, crust shed off and pinkish area appears. By day 28, the wound was healing leaving large scar. In animals of group B, on day 3, the wound was covered with brownish border having good granulation tissue. On day 7, the wound was more desiccated, completely brown in colour with thick granulation and size was nearly same. On day 14, wound contraction was very fast. On day 21, the crust detached off leaving a raw granular pinkish tissue. On day 28, the wound healed up completely by severe contraction leaving no scar. Normal epithelization with very good hair growth on wound area was observed on day 28, resembling normal skin (Figure: 5).
DISCUSSION
In the present study, one 20X20 mm2 square full-thickness skin (dorsal thoracic region) wounds were created on each of 18 adult wistar rats of either sex under standard anaesthetic protocol to evaluate the wound healing potential of medical grade chitosan powder in full thickness wounds in rats.
The animals of both groups remained dull on first postoperative day and assumed a hunched back posture, while resting in their cages. They started taking feed and water partially within 24h after surgery. In all the animals feed and water intake became normal by 3rd postoperative day. The animals of group B started the resting on dorsal recumbency from day 14, whereas, in group A, it was from day 21.These results were in accordance with other workers (Kaarthick, et al., 2011). It has been observed that the experimental animal (rat) generally rest in dorsal recumbency. The animals of group B started the resting on dorsal recumbency from day 14, whereas, in group A it was from day 21. It indicates the normalcy and healing was progressing well in the experimental group. Dullness, depression and partial anorexia observed in the immediate postoperative period (1 - 2 days) may be attributed to surgical trauma (pain) and inflammation at the site of reconstruction (Kaarthick, et al., 2011).
Significant (P < 0.05) increase in temperature for first 3 days post surgery was recorded in both groups which may be due to foreign body reaction, surgical trauma and stress to the animals following skin wound. The hyperthermia recorded in the early postoperative period started returning to normal as soon as the animals recovered from surgical stress. Pyrexia of variable degree in postoperative days has also been reported after the repair of full-thickness skin defects with different materials in rabbits (Gangwar et al., 2006; Purohit et al., 2008) and rats (Kaarthick, et al., 2011). The increase in temperature may also be attributed to the action of endogenous or leukocytic pyrogen produced by granulocytes, monocytes and macrophages (Atkins et al., 1960).
The warmth of the wounds was non -significantly lower up to day 3 post surgery. Similar findings have also been reported after the repair of full thickness skin defects with acellular matrix in rabbits (Purohit, 2008; Kumar, 2010) and in rats (Kaarthick et al., 2011). The vasodilatation of the local wound vessels leads to increased blood flow resulted in increase in the temperature of the wound on day 7 (Purohit et al., 2008).
Wound contraction has been used to monitor wound healing. Wound area decreased gradually as the healing progressed. The most important cell, the fibroblast attained the peak approximately on day 7 from injury and is responsible for initiating the angiogenesis, epithelialisation and collagen formation. Control wound healed completely by 28 days leaving a large scar indicating the existence of severe contraction. Chitosan group took 20 - 22 days for complete healing, but it was with minimum contraction leaving a little scar than control group. Wound contraction is the centripetal displacement of the wound edges that facilitates its closure after trauma. This process is carried out by myofibroblasts that contain α-actin from smooth muscle and is mediated by contractile forces produced by granulation tissue from wound (Neagos et al., 2006). Wound healing rate is defined as the gross epithelialisation of the wound bed. Wound contraction was assessed by percent retention of the original wound area (Schalleberger et al., 2008).
Moderate exudation at the site was observed upto day 3 - 5 in chitosan as well as control wounds. Exudation may be due to inflammatory reaction at the site in response to surgical trauma. As the healing progressed the inflammation subsided gradually and therefore, no exudation was observed on day 7 and onwards except in group A (control). A significant decrease in exudation after full-thickness wounds treated with small intestinal sub mucosa compared to untreated wounds in rat model was reported by (Kim et al., 2005). According to (Wang et al., 2007), a reverse correlation was detected between the survival area of the skin graft and the degree of exudation of the graft bed. Other workers also reported decrease in exudates from the full-thickness wounds repaired with acellular matrix in rabbit and rat model, as the healing progressed (Kaarthick et al., 2011).
Although moderate degree of postoperative pain was persisted up to day 6 in both the groups but pain scores was non-significantly (P > 0.05) higher within the group. In both the groups the pain scores reduced gradually and reached to minimum level at day 7. On day 3, animals of group A exhibited significantly higher pain, whereas, group B animals exhibited significantly lower value of pain due to less inflammatory response. Injury to tissue causes a number of changes in the nociceptive system. The injured nociceptors become highly sensitized to stimuli. Inflammatory mediators released during and after surgery also sensitized the peripheral nociceptors to further stimuli (Treede et al., 1992). Variation in duration of pain was due to surgical trauma and subsequently the extent of inflammation and tissue reaction. Higher degree of pain scores were also reported after the repair of full thickness skin defects in rabbits (Purohit et al., 2008) and in rats (Kaarthick et al., 2011).
Degree of peripheral swelling was found less in group B as compared to group A on day 3 and 7 post surgery. Degree of peripheral swelling was less in group B, because chitosan powder has anti-inflammatory and anti-bacterial action (Ishihara et al., 2002). Inflammatory mediators released during and after surgery also sensitized the peripheral nociceptors to further stimuli (Treede et al., 1992). The vasodilatation of the local wound vessels leads to increased blood flow resulted in increase in the swelling of the wound (Purohit et al., 2008).
Granulation tissue was first observed in group B on day 3 and in group A on day 4 post surgery. - In group A, granulation tissue was not so discernible by day 4, however, some areas of granulation tissue formation were observed towards the periphery. In group B, granulation tissue was formed below the skin edge between day 3 and day 7 and proliferated to the level of skin edges by day 7. On day 16 - 18, granulation tissue was almost fully covered the wound area in group B, whereas, wound area was covered by the granulation tissue in the control group (A) on day 21 - 22. Granulating tissue can generally be divided into two types, healthy and unhealthy granulating tissues. It is well known that healthy granulating tissue develops only in the absence of foreign bodies such as bacteria, debris, and so forth. Formation of healthy granulating tissue which is closely related to angiogenesis is a very important factor in wound healing (Clark and Denver et al., 1985). Granulation tissues with neo-vasculature were observed moderately at the site in contact with the chitin-sponge on day 7 and day 14 after the subcutaneous implantation of a sponge-like chitin in a dog (Okamoto et al., 1995). Similar finding was also found in this study in group B.
The color of the wound changed from white to dark brown and finally dark on subsequent time intervals. There was not so much difference in wound area of group A and B from day 0 to 3. On day 7; a layer of scar was present on both groups. There was drastic reduction in wound area from day 7 to day 14 in group B in comparison to group A. On day 20 - 22 healing was complete in group B leaving a very little scar, whereas, in control group (A) healing was complete in 27 - 28 days with abundant scar. Similar findings also have been reported after the repair of full thickness skin defects in rabbits (Purohit et al., 2008) and in rats (Kaarthick et al., 2011).
Full thickness skin wound healing occurs by granulation tissue formation, contraction and epithelialisation (Fossum et al., 2007). Epithelialisation occurs by migration of undamaged epidermal cells from the wound margins across the granulation bed (Swaim, Henderson et al., 1990). Exogenous collagen supplementation enabled faster migration of cells that are involved in cutaneous wound healing. Since the exogenous collagen is molecular in nature (Nithya et al., 2003) and supplies endogenous collagen in-vivo, it readily integrates with the wound tissue and facilitates the attachment, migration and proliferation of cells on the wound site (Judith et al., 2010).
Chitosan is biocompatible, biodegradable, haemostatic, anti-infective and more importantly, it accelerates wound healing (Ishihara et al, 2002). Porous chitosan scaffolds present a promising approach for tissue engineering applications (Hong-Ru et al., 2006). In experimental animal models, chitosan was shown to influence all stages of wound repair (Howling et al., 2001). The haemostatic activity of chitosan can be seen in the inflammatory phase. It also interacts and regulates the migration of neutrophils and macrophages acting on repairing processes such as fibroplasia and epithelialisation (Howling et al., 2001; Ishihara et al., 2002). Chitin and chitosan derivatives are well-tolerated, effective adjutants with considerable potential for clinical practice (Zaharoff et al., 2006). These reports further confirmed our observations that medical grade, sterilized chitosan powder are beneficial biomaterials and accelerated wound healing.
In conclusion, medical grade, sterilized chitosan powder showed better healing potentiality in comparison to standard dressing material (dermafin) for repair of full thickness skin wounds in rat model.
AKNOWLEDGEMENT
The authors are highly thankful to the Head, Division of Surgery and Director, Indian Veterinary Research Institute, Izatnagar, Uttar Pradesh, India for providing facilities to carry out this work.
CONFLIC OF INTEREST
The authors declare that they have no conflicts of interests with respect to their authorship or the publication of this article.
REFERENCES
Barrientos S, Stojadinovic O, Golinko MS, Brem H, and Tomic-Canic M (2008). Growth factors and cytokines in wound healing. Wound Repair Regen, 16: 585 - 601
http://dx.doi.org/10.1111/j.1524-475X.2008.00410.x
PMid:19128254
Bartone FF Adickes E (1988). Chitosan: effects on wound healing in aurogenital tissue: preliminary report. J Urol, 140:1134 - 1137
PMid:3184286
Bigbie RB, Schumacker J, Swaim SF, Purohit KC J.C., Wright JC (1991) Effect of amnion and yeast cell derivate on second intention healing in horses. Am J Vet Res., 52: 1376
PMid:1928923
Bohling MW, Henderson RA, Swaim SF, Kincaid SV, Wright JC (2004). Cutaneous wound healing in the cat: A Macroscopic description and comparison with cutaneous wound healing in the dog. Vet Surg, 33: 579 - 587
http://dx.doi.org/10.1111/j.1532-950X.2004.04081.x
PMid:15659012
Clark RAF, Denver MD (1985). Cutaneous tissue repair: Basic biologic considera¬tions. J Am Acad Dermatol, 13: 701 - 725.
http://dx.doi.org/10.1016/S0190-9622(85)70213-7
Conti B, Giunchedi P, Genta I, Conte U (2000). The preparation and in vivo evaluation of the wound-healing properties of chitosan microspheres. S T P Pharm Sci: 10, 101 - 104
Fossum TW, Hedlund CS, Johnson AL, Schulz KS, Seim HB, Wasard MD, Baer A, Carroll GL (2007). Surgery of Integumentary System. Manual of Small Animal Surgery, Mosby. pp. 159 - 175.
Gangwar AK, Sharma AK, Kumar N, Maiti SK, Gupta OP, Goswami TK, Singh R (2006). Acellular dermal graft for repair of abdominal wall defects in rabbits. J. South African Vet Assoc, 77: 79 - 85.
http://dx.doi.org/10.4102/jsava.v77i2.349
PMid:17120624
Gangwar AK, Naveen Kumar, Sharma AK, Devi S, Negi M, Shrivastava S, Mathew D, Remya V, Soanal, Arundeep PS, Maiti SK, Kumar V, Kaarthick DT, Kurade NP, Singh R (2013). Bioengineered acellular dermal matrix for the repair of full thickness skin wounds in rats. Trends Biomater Artif Organs, 27: 67 - 80.
Hong-Ru L, Ko-Shao C, Su-Chen C, Chih-Hung L, Shih-Hwa C, Ta-Li C, Te-Hsing W (2006). Attachment of stem cells on porous chitosan scaffold cross linked by Na5P3O10. Mat Sci Eng. C, 27: 280 – 284
Howling GI, Dettmar PW, Goddard PA, Hampson FC, Dornish M, Wood EJ (2011). The effect of chitin and chitosan on the proliferation of human skin fibroblasts and keratinocytes in vitro. Biomaterials, 22: 59 - 66
Ishihara M, Nakanishi K, Ono K, Sato M, Kikuchi M, Saito Y (2002). Photo cross linkable chitosan as a dressing for wound occlusion and accelerator in healing process. Biomaterials 23: 833 - 840
http://dx.doi.org/10.1016/S0142-9612(01)00189-2
Judith R, Nithya M, Rose C and Mandal AB (2010). Application of a PDGF-containing novel gel for cutaneous wound healing. Life Sci, 87: 1 -8
http://dx.doi.org/10.1016/j.lfs.2010.05.003
PMid:20470785
Kaarthick DT (2011). Repair of cutaneous wounds using acellular diaphragm and pericardium of buffalo origin seeded with in-vitro cultured mouse embryonic fibroblasts cells in rat model. M.V.Sc. Thesis submitted to Deemed University, I.V.R.I., Izatnagar, Bareilly (UP), India
Kim MS, Hong KD, H.W. HW, Kim SH, Kim SH, Lee MS, Jang WY, Khang G, Lee HB (2005). Preparation of porcine small intestinal sub mucosa sponge and their application as a wound dressing in full-thickness skin defect of rat. Int J Biol Macromole, 36: 54 – 60.
http://dx.doi.org/10.1016/j.ijbiomac.2005.03.013
PMid:15939465
Kumar V (2010). Acellular buffalo small intestinal sub mucosa and fish swim bladder for the repair of full thickness skin wounds in rabbits M.V.Sc. Thesis submitted to Deemed university, I.V.R.I., Izatnagar, Bareilly(UP) India
Nalbandian RM, Henry RL, Balko KW, Adams V, Neuman NR (1987). Pluronic F-127 gel preparation as an artificial skin in the treatment of third-degree burns in pigs. J. Biomed. Mater Res, 21: 1135 - 1148
http://dx.doi.org/10.1002/jbm.820210907
PMid:3667639
Neagos D, Mitran V, Chiraku G, Ciurab R, Lanku C, Stan C, Cimpean A, Iordachescu D (2006). Skin wound healing in a free floating fibroblast populated collagen lattice model. Romanian J Biophy, 16: 157 - 168
Nithya M, Suguna L, Rose C 2003). The effect of nerve growth factor on the early responses during the process of wound healing. Biochemica et Biophysica acta, 1620: 25 - 31
Okamoto Y, Minami S, Matsuhashi A, Tanioka S, Shigemasa Y (1995). The fate of N-acetyl-D-glucosamine (chitin) in canine subcutaneous tissues. SeitaiZairvo Biomaterials, 13: 112 - 116
Parameshwaraiah S, Shivakumar HG (1998). Evaluation of topical formulations of aqueous extracts of Centella asiatica on open wound in rats. Ind J Exp Biol, 36: 569 - 572
PMid:9731470
Purohit S (2008). Biocompatibility testing of acellular dermal grafts in a rabbit model: An in-vitro and In-vivo study. Ph.D. Thesis submitted to Deemed University, I.V.R.I., Izatnagar, Bareilly (UP)-243122, India
Schalleberger SP, Stanley BJ, Hauptman JG, Steficek BA (2008). Effect of porcine small intestinal submucosa on acute full-thickness wounds in dogs. Vet Surg, 37:515 - 524
http://dx.doi.org/10.1111/j.1532-950X.2008.00398.x
PMid:19134100
Snedecor GW, Cochran WG (1989). Statistical Methods, 8th Ed. Oxford and IBH Publishing Company, New Delhi
Swaim SF, Henderson RA (1990). Small Animal Wound Management, Lea and Febiger, Philadelphia, London. pp. 1 - 33.
Treede RD, Meyer RA, Raja SM (1992). Peripheral and central mechanisms of cutaneous hyperalgesia. Prog Neurobiol, 38: 397 - 421
http://dx.doi.org/10.1016/0301-0082(92)90027-C
Wang Y, Chen X, Armstrong MA, Gang L (2007). Survival of bone marrow derived mesenchymal stem cells in a xeno-transplantation model. J Ortho Res, 25: 926 - 932
http://dx.doi.org/10.1002/jor.20385
PMid:17415789
Wysocki AB (1999). Skin anatomy, physiology, and patho-physiology. Nurs Clin N Amm, 34: 777 - 797
PMid:10523436
Zaharoff DA (2006). Chitosan solution enhances both humoral and cell-mediated immune responses to subcutaneous vaccination Published online 2006 December. Vaccine, 2006.11.034