Advances in Animal and Veterinary Sciences
Research Article
Comparative Efficacy of Single and Double Layer Suturing along with Stapling Technique for End-To-End Anastomosis of Esophagus in Dog
Naveed Hussain1, Muhammad Ahmed Aleem Khadim1, Nasir Iqbal1*, Sadaf Aslam1, Ayesha Sadiq3, Zubair Luqman2, Hamza Jawad2
1Department of Veterinary Surgery and Pet Sciences, University of Veterinary and Animal Sciences, Lahore, Punjab, Pakistan; 2Faculty of Veterinary and Animal Sciences, The Islamia University of Bahawalpur, Bahawalpur, Punjab, Pakistan; 3Department of Pathology, University of Veterinary and Animal Sciences, Lahore, Punjab, Pakistan.
Abstract | The present-day study was carried out to compare the best surgical technique for end-to-end anastomosis of esophagus after resection. The clinical trials were carried out to compare three techniques for end-to-end anastomosis of esophagus which included single layer suturing, double layer suturing and stapling technique and various parameters were evaluated to compare their effectiveness at day 1, 3, 7, 15, 21, 28, 35 and 45 (physiological parameters, hematology, weight gain/loss, contrast radiography and endoscopy). The techniques were used in 12 mongrel dogs of either sex and divided into three groups A, B and C. It was concluded that stapling technique (intra luminal circular stapler 28mm) has been considered much better than other two techniques (Single layer Suturing and double layer suturing). The verdict base explanation for better and reliable result in esophageal anastomosis is that the stapling technique has good result in term of post-operative complications, less operative time; give more strength to the anastomosis ends of esophagus, good healing and minimum Stenosis.
Keywords | Esophagus, Single layer, Double Layer, Endoscopy and stenosis
Received | June 12, 2020; Accepted | June 22, 2020; Published | August 01, 2020
*Correspondence | Nasir Iqbal, Department of Veterinary Surgery and Pet Sciences, University of Veterinary and Animal Sciences, Lahore, Punjab, Pakistan; Email: Nasir.iqbal@uvas.edu.pk
Citation | Hussain N, Khadim MAA, Iqbal N, Aslam S, Sadiq A, Luqman Z, Jawad H (2020). comparative efficacy of single and double layer suturing along with stapling technique for end-to-end anastomosis of esophagus in dog. Adv. Anim. Vet. Sci. 8(9): 925-932.
DOI | http://dx.doi.org/10.17582/journal.aavs/2020/8.9.925.932
ISSN (Online) | 2307-8316; ISSN (Print) | 2309-3331
Copyright © 2020 Hussain et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Esophagus is an important part of the gastrointestinal tract. It starts as a downward prolongation of pharynx in the neck, originating from the caudal border of the laryngeal cricoid cartilage approximately at the level of sixth cervical vertebra. The esophagus consists of cervical, thoracic and abdominal portions (Osborne et al., 1967). At its origin the esophagus lies dorsal to trachea. The cervical part progressively shows left decline and lies on the left of the trachea till thoracic inlet, afterwards the thoracic part takes turn to dorsal aspect of trachea and remains in this position till tracheal bifurcation. Then esophagus enters the abdominal cavity via diaphragm (esophageal hiatus) where it attaches to cardia of the stomach (Zboralske and Friedland, 1970). Cranial and caudal thyroid arteries supply blood to the cranial part of the esophagus while esophageal branches of gastric artery supply the thoracic part (Liebermann-Meffert, 2001). Innervations to the esophagus are provided parasympathetically from vagus nerve.
The cervical esophagus is composed of four tunics i.e. adventitia, muscularis, sub-mucosa and mucosa (Watson, 1974). Tunica adventitia is the thin outer fibrous membrane consists of loose connective tissue which connects the esophagus with adjoining structures. It comprises of nerve fibers, tiny vessels and lymphatics. The muscularis consists of two muscle layers of the fibers which are striated in nature and arranged perpendicularly. Sub-mucosa is elastic and collagenous layer, present between muscular coat and the mucosa, which forms a network of nerves, mucous glands, lymph and blood vessels, Mucosa is comprised of three parts, tunica propria, the muscularis mucosae, which is enriched with small lymph vessels present near the border of sub-mucosa and stratified squamous non-keratinized epithelium (Debas, 2004).
There may be multiple causes for esophageal obstruction i.e. trauma, Scar tissue, esophageal tumors and stricture. Esophageal foreign bodies are a common emergency problem in veterinary practice which may lead to necrosis with time (Sale and Williams, 2006). These foreign bodies can trap at any place in the esophagus, but narrow positions are more predilection sites (Rousseau et al., 2007). Esophageal obstruction is presented with acute signs of gagging, coughing, regurgitation, ptyalism, vomiting and dysphagia (Luthi and Neiger, 1998). Complications linked with esophageal obstruction include esophageal tear, aspiration pneumonia, esophageal stricture formation and esophagitis (Tams, 2003) which may lead to necrosis. Esophageal resection and anastomosis may be required as corrective surgery in number of esophageal obstruction cases. Various techniques may be applied for end-to-end anastomosis of esophagus including single layer closure, double layer closure and surgical staples. In single layer technique all four layers of esophagus are sutured in a single row by using appropriate absorbable suture material with simple interrupted suture pattern in which knots are kept extraluminal (Ranen et al., 2004).
In double layer technique the anastomosed ends of esophagus are closed in two rows i.e. tunica mucosa and sub-mucosa are sutured in one layer by using simple interrupted suture pattern in which knots are kept intra-luminal, while tunica muscularis and adventitia are sutured as second layer by using interrupted pattern and knots are kept extra-luminal. The use of mechanical stapling devices for gastrointestinal anastomosis are in practice in veterinary and human esophageal surgery to reduce anesthesia and operating time Circular staplers are popular for this purpose. These staplers are used for apposition of anastomosed esophageal ends (Laterza et al., 1999). Selection of the stapler is based on the diameter of the esophageal lumen and thickness of the esophageal wall (Zhang et al., 2018). Commonly 24, 26 and 28mm circular staplers are selected for esophageal anastomosis. Staplers present an accurate, secure and consistent mechanical apposition of anastomosed tissues (Belandria et al., 2009).
So, the current project was designed to assess comparative efficacy of three different closure techniques for end to end anastomosis in terms of easy and reliable approach with special emphasis on the effectiveness of the Procedures, improving diameter of esophagus Perforation/necrosis and least post-operative complications of the procedures used.
MATERIALS AND METHODS
Animal selection
The present study was conducted on 12 adult mongrel dogs of either sex or breed, six months to 3 years of age with an average body weight of 20 to 40 kg. The dogs were further divided into 3 groups named as group A, B and C. Almost 10 days prior to initiation of surgery all dogs were acclimatized in the kennels at Surgery Section, Department of Clinical Medicine and Surgery, University of Veterinary and Animal Sciences, Lahore for complete examination as standard procedure and to make them familiar with the environment.
Table 1: White blood cells values in group A, B and C.
| Days |
White Blood Cell (103/μl) |
||
| Group A | Group B | Group C | |
| Mean ± S.D | Mean ± S.D | Mean ± S.D | |
| 1 | 11.2 ± 5.6 | 11.4 ± 6.5 | 10.4 ± 2.8 |
| 3 | 17.0 ± 5.4 | 13.2 ± 6.0 | 11.0 ± 3.1 |
| 7 | 20.5 ± 6.2 | 15.9 ± 7.5 | 11.4 ± 3.9 |
| 15 | 24.4 ± 6.3* | 17.4 ± 11.0 | 12.1 ± 4.1 |
| 21 | 24.5 ± 8.9* | 16.9 ± 10.5** | 12.2 ± 4.6 |
| 28 | 25.5 ± 9.1 | 16.2 ± 9.8 | 11.9 ± 4.2 |
| 35 | 23.2 ± 6.7 | 18.3 ± 11.5 | 12.4 ± 4.2 |
| 45 | 16.0 ± 2.8 | 18.8 ± 11.1 | 12.5 ± 4.0 |
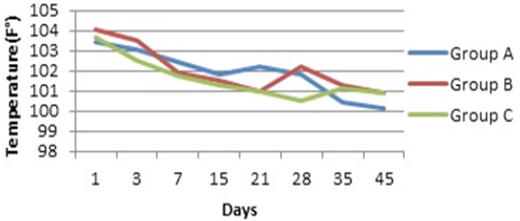
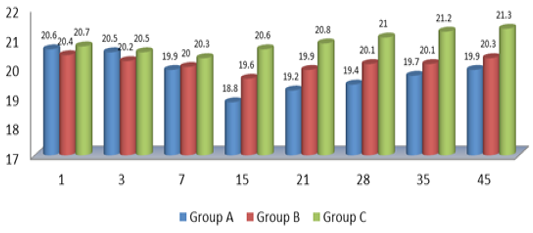
Figure 1: Comparative Mean Values of Temperature
Pre-operative clinical examination
All the animals underwent a thorough physical examination and complete blood count prior to start of study to rule out any pre-operative problems. The dogs were examined and treated for the possible external and internal parasitic infestations. Bath with “Hartz” dog shampoo was given prior to surgery to get rid of dirt and external parasites. Deworming was done with “Caniverm” tablet (Fenbendazolum 150 mg, Pyranteli embonas 144 mg, Praziquantelum 50 mg) at the dose rate of 1 tablet for 10 kg live body weight. All dogs were vaccinated by using RABISIN® 1ml subcutaneously as prophylactic measure (Touihri et al., 2011). Five days prior to surgeries, dogs were injected with broad spectrum antibiotics to minimize the risk of any systemic infection. During the whole study period, animals were housed in the available research facilities at Surgery Section, Department of Clinical Medicine and Surgery, University of Veterinary and Animal Sciences, Lahore.
Table 2: Red blood cells values in group A, B and C.
| Days |
Red Blood Cell(106/μl) |
||
| Group A | Group B | Group C | |
| Mean ± S.D | Mean ± S.D | Mean ± S.D | |
| 1 | 5.9 ± 0.9 | 5.0 ± 1.5 | 6.8 ± 0.5 |
| 3 | 6.6 ± 1.0 | 5.4 ± 1.1 | 6.7 ± 0.4 |
| 7 | 6.6 ± 1.0 | 5.5 ± 1.0 | 6.5 ± 0.6 |
| 15 | 6.3 ± 0.6* | 5.7 ± 0.8 | 6.5 ± 0.9 |
| 21 | 6.7 ± 0.6* | 5.8 ± 1.1** | 6.7 ± 0.6 |
| 28 | 7.0 ± 0.7 | 6.4 ± 0.8 | 6.7 ± 0.6 |
| 35 | 6.5 ± 0.4 | 6.7 ± 0.9 | 7.2 ± 0.9 |
| 45 | 6.0 ± 0.0 | 6.9 ± 0.5 | 7.1 ± 0.9 |
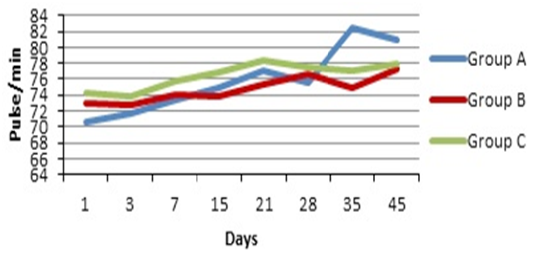
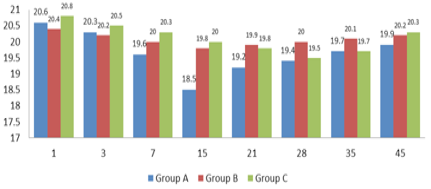
Figure 2: Comparative Mean Values of Pulse
Premedication and anesthesia
All the dogs were given a pre-anesthetic dose of Xylazine hydrochloride (Xylaz, Farvet) at the dose rate of 0.1- 1 mg/kg intra muscular (Slatter, 2003). The dogs were sedated by using combination of Xylazine + Ketamine and Atropine sulphate (2.2mg/kg + 10-15mg/kg + 0.04mg/kg respectively) administered intramuscularly. Maintenance of anesthesia was achieved by intravenous administration of propofol @ 1-2.5 mg/kg (Gobifol) (Kharasch et al. 1995). Intravenous fluids (Dextrose 5% Solution) and injection Transamine @ 10-20mg/kg as intravenous haemostatic agent were administered during surgery.
Surgical procedure
The standard surgical procedure for esophageal resection and anastomosis was performed as following:
Surgery for esophageal resection
A gastric tube was passed via oral route for identification of esophagus for resection purposes. For surgery the cervical esophagus was approached by ventral midline incision. The incision (approximately 8 to 10 cm) was made from larynx towards manubrium, incising skin and subcutaneous tissue with scalpel blade No. 24. The undermining was done by blunt dissection throughout the length of incision. Platysma muscle and subcutaneous tissues were incised and retracted. The sternohyoid muscles and sternocephalicus muscles were separated and retracted. The trachea was retracted to the right to expose the esophagus and adjacent structures including thyroid gland, thyroid vessels, recurrent laryngeal nerve and carotid sheath. The intubated esophagus was isolated with moistened laparotomy sponges and, stay sutures were applied for gentle tissue handling and maintaining configuration. The lumen was occluded with non-crushing clamp and 2cm portion of esophagus was resected.
Table 3: Haemoglobin values in group A, B and C.
| Days | Haemoglobin (g/dl) | ||
| Group A | Group B | Group C | |
| Mean ± S.D | Mean ± S.D | Mean ± S.D | |
| 1 | 11.3 ± 3.8 | 12.7 ± 4.5 | 14.8 ± 2.1 |
| 3 | 10.5 ± 3.8 | 11.2 ± 4.0 | 14.3 ± 1.3 |
| 7 | 11.0 ± 4.8 | 10.0 ± 5.0 | 13.4 ± 0.7 |
| 15 | 11.6 ± 5.4* | 10.6 ± 5.7 | 13.5 ± 0.8 |
| 21 | 10.9 ± 6.6* | 11.8 ± 6.2** | 14.2 ± 0.8 |
| 28 | 10.3 ± 5.4 | 12.3 ± 7.4 | 14.8 ± 0.3 |
| 35 | 11.7 ± 6.3 | 11.9 ± 7.0 | 15.0 ± 0.8 |
| 45 | 11.8 ± 6.9 | 12.1 ± 7.0 | 15.8 ± 1.0 |
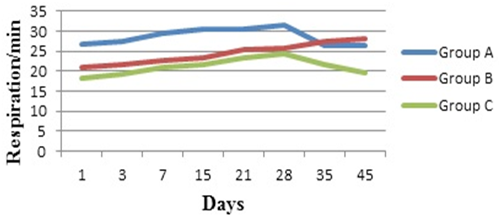
Figure 3: Comparative Mean Values of Respiration
End-to-end anastomosis closure techniques
After resection of esophagus end-to-end anastomosis was achieved in following manner.
Group A: Esophagus was sutured by using single layer closure technique i.e. simple interrupted suture pattern was used by using 2/0 chromic catgut. All four layers of esophagus mucosa, sub-mucosa, muscularis and adventitia were incorporated. The knots were kept extraluminal.
Group B: Esophagus was sutured by using Double layer closure technique. Simple interrupted suture pattern was used by using 2/0 chromic catgut. All four layers of esophagus were closed in two layers. The mucosa and sub-mucosa were sutured as one layer by using simple interrupted suture pattern and the knots were kept intra-luminal. The muscularis and adventitia were sutured as second layer by using simple interrupted suture pattern and the knots were kept extra-luminal.
Group C: Esophagus was closed by stapling technique i.e. intra luminal circular stapler 28mm was used for closure. Covidien Premium Plus CEEA TM 28 stapler holds a circular, double staggered row of titanium staples. Covidien Premium Plus CEEA TM stapler comprised of a circular anvil, cartridge (which contains rows of staples) and circular knife. For anastomosis purpose purse string sutures were applied on both resected ends of esophagus. Stapler anvil was separated from the cartridge by rotating adjustable nut anti-clockwise and then inserted into the lumen of distal resected esophageal end. Purse string sutures of distal end were tightened, leaving anvil pin outside of lumen. The cartridge was introduced via oral route to the proximal resected end and sutures were tightened as above with cartridge pin outside of lumen. Then resected esophageal ends were apposed by closing the anvil against cartridge and rotating the adjustable nut clockwise. End-to-end anastomosis of esophagus was achieved by removing the safety valve and pressing the handle of stapler to fire the staples. Circular knife helped to remove extra esophageal intra-luminal mass during procedure.
Table 4: Erythrocyte sedimentation rate values in group A, B and C.
| Days | ESR (mm/h) | ||
| Group A | Group B | Group C | |
| Mean ± S.D | Mean ± S.D | Mean ± S.D | |
| 1 | 9.0 ± 0.1 | 7.0 ± 0.2 | 6.0 ± 0.2 |
| 3 | 10.0 ± 0.2 | 9.0 ± 0.3 | 7.0 ± 0.2 |
| 7 | 11.0 ± 0.1 | 8.0 ± 0.2 | 6.0 ± 0.3 |
| 15 | 13.0 ± 0.1* | 10.0 ± 0.1 | 5.0 ± 0.3 |
| 21 | 9.0 ± 0.1* | 6.0 ± 0.3 ** | 4.0 ± 0.2 |
| 28 | 8.0 ± 0.2 | 5.0 ± 0.2 | 4.0 ± 0.1 |
| 35 | 7.0 ± 0.2 | 4.0 ± 0.3 | 3.0 ± 0.4 |
| 45 | 6.0 ± 0.2 | 3.0 ± 0.3 | 5.0 ± 0.1 |
Evaluation of end-to-end anastomosis closure techniques
Following parameters were used in the experiment for comparison of techniques at days 1, 3, 7, 15, 21, 28, 35 and 45 post-surgery.
Physical evaluation
Dogs were kept under observation for physical parameters including TPR (rectal temperature, pulse and respiration), feed and liquid intake, subcutaneous emphysema, weight gain/loss, vomiting and swallowing difficulty. Accurate Plus scale system® Yaohua YH-T6B was used for weight measurement.
Hematological evaluation
The blood sample (1ml) was collected in a vacutainer containing an anticoagulant (K2 EDTA) from the cephalic vein of dog. The blood sample was sent to University Diagnostic Lab (UDL), University of Veterinary and Animal Sciences, Lahore for complete hematological analysis. Complete blood count was performed by using Hematology Veterinary Analyzer (Abacus Junior Vet CBC Analyzer 2001) to evaluate infection, blood loss/anemia etc.
Table 5: Wound healing in group A, B and C.
| Days | Wound Healing (Endoscopy) | |||||||||||
|
Group A |
Group B |
Group C |
||||||||||
| A1 | A2 | A3 | A4 | B1 | B2 | B3 | B4 | C1 | C2 | C3 | C4 | |
| 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 3 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 7 | 2 | 1 | 1 | 1 | 1 | 2 | 1 | 2 | 2 | 2 | 2 | 2 |
| 15 | 2 | E | 2 | 1 | 1 | 2 | 1 | 2 | 2 | 3 | 2 | 3 |
| 21 | 2 | E | 2 | E | E | 3 | 2 | 2 | 3 | 3 | 3 | 3 |
| 28 | 2 | E | 2 | E | E | 3 | 2 | 3 | 3 | 3 | 3 | 3 |
| 35 | 2 | E | 2 | E | E | 3 | 2 | 3 | 3 | 3 | 3 | 3 |
| 45 | 3 | E | 3 | E | E | 3 | 3 | 3 | 3 | 3 | 3 | 3 |
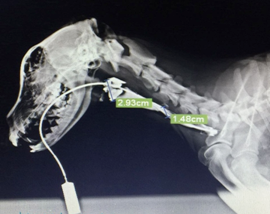
Contrast radiography
Contrast radiographs were taken by using Urografin 20ml having barium sulphate @ 6-12ml/kg (E-Z-HD 98% w/w) at Pet Centre, University of Veterinary and Animal Sciences, Lahore. Thick barium solution was administered orally by using 50 ml syringe under sedation. Serial radiographs were taken by using digital x-ray machine (Collimator Type R-20J 2015 SHIMADZU CORPORATION) for evaluation of esophageal perforation.
Table 6: Leakage evaluation (Endoscopy) in group A, B and C.
|
Days
|
Leakage Evaluation (Endoscopy) | |||||||||||
|
Group A |
Group B |
Group C |
||||||||||
| A1 | A2 | A3 | A4 | B1 | B2 | B3 | B4 | C1 | C2 | C3 | C4 | |
| 1 | A | A | A | A | A | A | A | A | A | A | A | A |
| 3 | A | P | A | A | A | A | P | A | A | A | A | A |
| 7 | A | P | A | P | A | A | A | A | A | A | A | A |
| 15 | A | E | A | P | P | A | A | A | A | A | A | A |
| 21 | A | E | A | E | E | A | A | A | A | A | A | A |
| 28 | A | E | A | E | E | A | A | A | A | A | A | A |
| 35 | A | E | A | E | E | A | A | A | A | A | A | A |
| 45 | A | E | A | E | E | A | A | A | A | A | A | A |
Endoscopy
Endoscopy was performed in dogs under sedation by using PENTAX EG-290 Kp 2015 Endoscope at Pet Centre, University of Veterinary and Animal Sciences, Lahore for the evaluation of esophageal stenosis, healing and perforation.
Statistical analysis
The obtained data was primarily organized by Mean±S.E.and lateranalysed by using Analysis of Variance (ANOVA) with the help of Minitab software (version.16).
Ethical consideration
This study was carried out following the rules and regulation approved by Ethical Review Committee (ERCULA), University of Veterinary and Animal Sciences, Lahore.

Figure 7: Endoscopic View of Esophagus
RESULTS
Physical evaluation
Temperature
Statistical analysis showed P-Value P=0.2 which indicates non-significant difference between groups
Pulse
The calculated P-Value of Pulse showed non-significant difference among all three groups.
Respiration
P-value showed non-significant difference between groups.
Hematological parameters
White blood cells
* Dogs expired during experiment: Statistical analysis showed P-Value (0.01) indicating significant difference between groups. Values of group A indicate occurrence of infection in animals, while group C was least exposed to infection during post-operation.
Red blood cells
* Dogs expired during experiment: On statistical analysis, P-Value (0.003) shows significant differences between groups. Animals of group C, showed less blood loss from incision site post-operation and prompt recovery. In group B, the situation was better than group A but less then grou.
Hemoglobin
* Dogs expired during experiment: On statistical analysis P-Value (0.001) shows significant difference between groups. Animals of group C, showed less blood loss, prompt recovery and better health status with more nutritional and oxygen supply to incision site. In group B, the situation was better than group A but less then group C.
Erythrocyte sedimentation rate
* Dogs expired during experiment: Statistical analysis showed P-Value (0.00) indicating significant difference between groups. Values of group A indicate occurrence of infection in animals as compare to group B, while group C was least exposed to infection during post-operation.
Body weight (In Kg)
Body Weight of dogs was observed at different days from day 1 to day 45 in all groups. Statistical analysis showed P-Value P= 0.001 which indicates significant difference between groups. Dogs of group C gained some weight after recovery, but weight of group B and C was not increased.
Contrast radiography
Lumen diameter of esophagus
Statistical analysis showed P-Value = 0.00 which indicate significant difference between groups. It shows variation in Post-operative luminal diameter of esophagus of group A, B and C. Narrowing of lumen/stricture was pronounced in group A, moderate in group B while least in group C.
Endoscopy
Wound healing
E = expired
1 = Poor Healing
2 = Moderate Healing
3 = Good Healing
Endoscopy revealed that in group A all dogs showed poor to moderate healing, in group B it was moderate to good while in group C healing was good in all animals.
Leakage evaluation (Endoscopy)
E = expired
Group A: Endoscopy showed leakage in 2 dogs (A2, A4), which expired later even after surgical intervention. Group B: Leakage was observed in 2 dogs (B1, B3), one dog (B3) survived and other (B1) expired after resuturing. Group C: All dogs survived till end of experiment and no leakage was observed.
DISCUSSION
The present study was carried out to compare the best surgical technique for end-to-end anastomosis of esophagus after resection (Slatter, 2003).Esophageal reconstruction is indicated in different pathological conditions like esophageal stenosis, tumors, trauma, foreign bodies, diverticulum, mega esophagus and esophageal motility disorders. The clinical trials were carried out to compare three techniques for end-to-end anastomosis of esophagus which included single layer suturing, double layer suturing and stapling technique and various parameters were evaluated to compare their effectiveness at day 1, 3, 7, 15, 21, 28, 35 and 45.The topographic approach of esophagus denoted in current study was similar to that stated by (Liebermann‐Meffert, 2001).
Temperature, pulse and respiration were checked to evaluate general health status which indicated insignificant difference between groups. Graphical presentation of these parameters coincided with (Maish et al., 2005). Various hematological parameters were analyzed to determine effects of esophageal resection on overall body health. There was significant difference between groups in terms of WBCs, RBCs, Hb and ESR. The level of white blood cells elevated initially in group A and B and then gradually decline till end of experiment, whereas least change was observed in group C as compared to group A and B. RBCs and Hb values were at slightly reduced level then normal in group A and B which revealed slight blood loss, reduced local nutritional and oxygen supply post-surgery, while in group C values were in normal range and consistent throughout the experiment. Values of ESR were highly elevated in group A, less in group B and least in group C which indicated presence of high levels of infections and inflammatory changes respectively. These hematological parameters were agreed with that denoted by (Chao et al., 2010) and (Ranen et al., 2004).
Post-surgery, animals were kept off-feed and water for first five days and nutritional supplementation was given by IV line. After 5th day liquid diet was started which was gradually replaced with semisolid and later with solid one with progression of time. Liquid and food intake was least initially in all groups which progressively improved with time. In group wise, overall it was noted that there was minor food and liquid intake in group A, minor to normal in group B and normal in group C from initiation of feed to end of experiment. These results are coincided with that described by (Viklund et al., 2006).
Clinical evaluation of esophageal perforation/stenosis was done by evaluating the frequency of vomiting, subcutaneous emphysema and swallowing difficulty. In average these signs were overall severe in group A, moderate in group B and least in group C which coincided with the findings of (Viklund et al., 2006). Gain/loss in body weight revealed that there was significant difference between groups. Group C showed slight better weight gain till end of experiment whereas no weight gain was observed in group A and B.
Contrast radiography was used to evaluate luminal diameter/stenosis and leakage at surgical site which revealed that there was significant difference in luminal diameter between groups. Marked decrease in diameter was observed in group A, moderate in group B, while least in group C. These results were similar to that reported by (Serhal et al., 2010) and (Boone et al., 2008). As far as leakage is concerned, radiography revealed that leakage in group A outnumbered group B, while no leakage was seen in group C. These findings were agreed with findings of (Bladergroen et al., 1986). Endoscopy was used to observe level of wound healing and perforations. Wound healing at different experimental intervals revealed that in group A healing was poor, in group B it was moderate to good and in group C it was good to excellent. These findings were agreed with (Hsu et al., 2004). The perforation/leakage evaluation showed that number of perforations was marked in group A, less in group B and none in group C. These endoscopic findings were similar as described by (Hogan et al., 2008).
It was concluded that stapling technique (intra luminal circular stapler 28 mm) has been considered much better then the other two techniques (single layer suturing and double layer suturing). The verdict base explanation for better and reliable result in esophageal anastomosis is that the stapling technique has good results in term of post-op complication, less operative time, give more strength to the anastomosed ends of esophagus, good healing and minimum stenosis. According to our findings double layer suturing technique may be considered as second option due to minimum chances of perforation along with mild fibrosis and stenosis with good healing time. Single layer suturing technique may be third one and least accepted because it experiences more post-op complications, greater chances of infection, dehiscence of anastomosed ends due to less strength and increased stenosis levels.
Authors Contribution
Muhammad Ahmad Aleem Khadim, Nasir Iqbal, Sadaf Aslam and Naveed Hussain: Research Trial and Revision. Ayesha Sadiq, Zubair Luqman and Hamza Jawad: Formatting and Setting.
Conflict of interest
The authors have declared no conflict of interest.
REFRENCES