South Asian Journal of Life Sciences
Research Article
Study on Binocular Vision Assessment and Refraction in Patients of Anterior Segment Corneal Dystrophies: The Pakistani Hospital Based Study
Shagufta Naz*, Ahlam Munsif Butt, Saima Sharif, Farzana Rashid, Tasnim Farasat
Department of Zoology, Lahore College for Women University, Jail Road Lahore.
Abstract | The aim of this research was to determine the characteristics of refraction associated with Anterior Corneal Dystrophies (ACDs). Present retrospective, analytical study was performed between October 2012 and June 2013 on all cases seen from different cities of Punjab during ophthalmological consultation at the Layton Rahmatullah Benevolent trust hospital, Mughal Eye Hospital & General Hospital. The techniques used for the diagnosis of Anterior Corneal Dystrophies were an examination of cornea using a slit lamp biomicroscope, topography, orbscan, keratometry, phoropter and far visual acuity. Indeed a drop in visual acuity and blindness were the main reasons for consultation in this study. Fifty three cases of ACDs were identified from Punjab, corresponding to hospital prevalence of 0.5/1000. The ACDs were studied in 13 women and 40 men. ACDs are predominant in age group 11-20 years. The chi-square test was used for comparison between different age groups and was considered significant at P < 0.05. The variables examined were age, gender, main complaint and far visual acuity. No association was found among any of the variables. Anterior Corneal Dystrophies leads to much decreased vision due to refractive errors and in some cases to corneal blindness with marked variation in phenotypes. Each Corneal Dystrophy needs elaborative study to find out the pathology of each dystrophy precisely. Affected families should be examined and interrogated to determine the site of mutation within their genome and the consequences causing these mutations. Different aids should be developed for decreasing visual disability of the affected individuals.
Keywords | ACD = Anterior Corneal Dystrophy, CCT = Central Corneal Thickness, CD = Corneal Dystrophy, CF = Counting Fingers, HM = Hand Movement
Editor | Muhammad Nauman Zahid, Quality Operations Laboratory, University of Veterinary and Animal Sciences, Lahore, Pakistan.
Received | February 02, 2015; Revised | February 27, 2015; Accepted | February 28, 2015; Published | March 07, 2015
*Correspondence | Shagufta Naz, Lahore College for Women University, Lahore, Pakistan; Email: shagufta502@yahoo.com
Citation | Naz S, Butt AM, Sharif S, Rashid F, Farasat T (2015). Study on binocular vision assessment and refraction in patients of anterior segment corneal dystrophies: the Pakistani hospital based study. S. Asian J. Life Sci. 3(1): 1-5.
DOI | http://dx.doi.org/10.14737/journal.sajls/2015/3.1.1.5
ISSN | 2311–0589
Copyright © 2015 Naz et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
INTRODUCTION
Visual perception is a main characteristic of the living beings by using it they can interpret the surrounding environment and process the information that is contained in visible light. The resulting perception is referred to as eyesight or vision. The visual system includes the various physiological components involved in vision. Visual impairment is referred to as the functional loss of the vision.
According to the fact sheet N°282 June 2012, provided by World Health Organization (WHO) the major causes of visual impairment are:
Refractive errors arise due to changes in the cornea or lens. Rare diseases, associated with degeneration and alteration of cornea are termed as Corneal Dystrophies. Corneal Dystrophies (CDs) are a group of genetic eye disorders which progresses slowly and leads to accumulation of abnormal material in the transparent cornea. Corneal Dystrophies are inherited bilateral, primary alterations of the cornea which are not associated with any symptoms as the disease initiates (Fujiki et al. 2001). CDs may be asymptomatic in some individuals whereas in others they may cause significant vision impairment. The age of onset and specific symptoms vary among the different forms of CDs. Most forms of corneal dystrophies have some similar characteristics i.e. they affect both eyes, progress slowly, do not affect other areas of the body and tend to run in families. It may be inherited as autosomal dominant traits, autosomal recessive traits, X-linked recessive or mitochondrial recessive traits and sporadic.
Anterior Corneal Dystrophies affect the outer layers of the cornea including the epithelium, the epithelial basement membrane that is a thin membrane that separates epithelial cells from underlying tissue, and the Bowman membrane (Klintworth, 2009). Commonly CDs have are accompanied by an initial symptom known as a ‘foreign body’ sensation. This is caused by breakdown of the surface epithelial layer. Sensitive nerve endings of the eye are exposed as the dystrophy causes a change in the outermost epithelial layer.
A retrospective, analytical study was performed between October 2012 and July 2013 on all Anterior Corneal Dystrophy (ACD) patients visiting LRBT, General Hospital and Mughal Eye Hospital from different areas of Punjab Province during their ophthalmic consultation. The aim of this research was to determine the significance of visual impairment associated with ACD patients due to errors in the refractive power of the anterior segment of cornea.
MATERIALS AND METHODS
Patients affected with Anterior Corneal Dystrophies were searched by visiting the Layton Rahmatullah Benevolent Trust hospital, General Hospital and Mughal Eye Hospital. Performas to get preliminary information about the postal address, diagnosis and disease status in the patients were filled out by inquiring the patients of Cornea in the hospital.
Case files of patients with ACDs were assessed to analyze:
The diagnosis of Anterior Corneal Dystrophies was made on the basis of an assessment of
Statistical Analysis
Data collected were arranged. The chi-square test was used for comparison between different age groups and was considered significant at P < 0.05. The variables examined were age, gender, main complaint and far visual acuity.
RESULTS
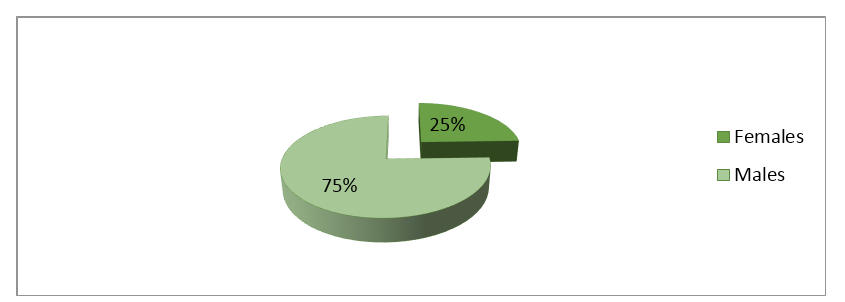
Among the 10000 patients studied from different cities of Punjab, 53 cases of Anterior Corneal Dystrophies were recognized which included 24.53% (13 cases) females and 75.47% (40 cases) males (Figure 1). One hundred and six eyes of 53 patients were assessed; 26 of females and 80 of males (Table 1). ACDs were found to be bilateral in 84.90% (45 cases) which included 22.64% (12 females) and 62.26% (33 males) and isolated in 15.09% (8 cases) comprising of only 0.01% (1 case) female and 13.20% (7 cases) males. Average age was found to be 19.56 with a range of 6-45 years. The most represented age group was 11-20, which included 64.15% (34 cases) patients, followed by patient aged 21-30 years including 18.86% patients (10 cases). There were 9.43% (5 cases) patients in the age group of 31-40, 1.90% (1 patient) > 40 years and 3.80% (2 patients)<10 years (Table 2).
Table 1: Crude prevalence of visual disability in 106 eyes of patients of ACDs
|
Snellen Eq. (Feet) |
SnellenEq. (Meters) |
N |
% |
|
20/20 |
6/6 |
9 |
8.50 |
|
20/30 |
6/9 |
2 |
1.90 |
|
20/60 |
6/18 |
4 |
3.77 |
|
20/80 |
6/24 |
2 |
1.90 |
|
20/137 |
6/36 |
7 |
6.60 |
|
20/183 |
6/48 |
1 |
0.94 |
|
20/200 |
6/60 |
12 |
11.32 |
|
20/2000 † |
6/600 |
52 |
49.05 |
|
20/20,000 § |
6/6000 |
12 |
11.32 |
|
Perception of light |
PL |
4 |
3.77 |
|
No perception of light |
NPL |
1 |
0.94 |
|
TOTAL |
106 |
100 |
N= number of eyes; †= counting fingers; §= hand Movement
Table 2: Age distribution of patients of ACDs by gender
|
Age |
F |
% |
M |
% |
N |
% |
|
< 10 |
0 |
0.00 |
2 |
5.00 |
2 |
3.80 |
|
11-20 |
8 |
61.53 |
27 |
67.5 |
35 |
66.03 |
|
21-30 |
2 |
15.40 |
8 |
20.0 |
10 |
18.90 |
|
31-40 |
2 |
15.40 |
3 |
7.50 |
5 |
9.43 |
|
> 40 |
1 |
7.70 |
0 |
0.00 |
1 |
1.90 |
|
Total |
13 |
100 |
40 |
100 |
53 |
100 |
F= number of females; M= number of males; N= total number of patients
Table 3: Age distribution of Myopia in the patients of ACDs
|
Age |
F |
% |
M |
% |
N |
% |
|
< 10 |
0 |
0.00 |
0 |
0.00 |
0 |
0.00 |
|
11-20 |
2 |
100.0 |
12 |
75.0 |
14 |
77.78 |
|
21-30 |
0 |
0.00 |
4 |
25.0 |
4 |
22.22 |
|
31-40 |
0 |
0.00 |
0 |
0.00 |
0 |
0.00 |
|
> 40 |
0 |
0.00 |
0 |
0.00 |
0 |
0.00 |
|
Total |
2 |
100 |
16 |
100 |
18 |
100 |
F= number of females; M= number of males; N= total number of patients
Table 4: Age distribution of Hyperopia in patients of ACDs
|
Age |
F |
% |
M |
% |
N |
% |
|
< 10 |
0 |
0.00 |
1 |
25.00 |
1 |
16.67 |
|
11-20 |
0 |
0.00 |
3 |
75.0 |
3 |
50.0 |
|
21-30 |
0 |
0.00 |
0 |
0.00 |
0 |
0.00 |
|
31-40 |
1 |
50.00 |
0 |
0.00 |
1 |
16.67 |
|
> 40 |
1 |
50.00 |
0 |
0.00 |
1 |
16.67 |
|
Total |
2 |
100 |
4 |
100 |
6 |
100 |
F= number of females; M= number of males; N= total number of patients
Table 5: Age distribution of Astigmatism in patients of ACDs
|
Age |
F |
% |
M |
% |
N |
% |
|
< 10 |
0 |
0.00 |
0 |
0.00 |
0 |
0.00 |
|
11-20 |
1 |
100.0 |
7 |
77.78 |
8 |
80.0 |
|
21-30 |
0 |
0.00 |
1 |
11.11 |
1 |
10.0 |
|
31-40 |
0 |
0.00 |
1 |
11.11 |
1 |
10.0 |
|
> 40 |
0 |
0.00 |
0 |
0.00 |
0 |
0.00 |
|
Total |
1 |
100 |
9 |
100 |
10 |
100 |
F= number of females; M= number of males; N= total number of patients
Main complaint was drop in visual acuity which was found in all the patients (100%). Factors responsible for decreased visual acuity were Corneal opacity which occurred in 56.60% (30 cases; 9 females and 21 males); keratoconus in 56.60% (30 patients; 4 females and 26 males) and nystgamus in 7.54% (4 persons; 2 of females and 2 of males). Munson sign was found to be positive in 24.52% (13 patients) cases, all of which were males whereas Oil droplet sign was also found positive in 24.52% (13 cases) but one of them was female. Acute hydrops was reported in only 3.77% (2 cases; one male and one female). Disease was found to be accompanied by pain in 13.20% patients (7 cases of which 3 were females and 4 were males). Myopia was found in 33.96% (18 cases), hyperopia in 11.32% (6 cases) and astigmatism in 18.86% (10 cases) (Table 3, 4, 5 and 6). Error was recorded in 35.84% due to excessive damaged cornea. Of the total patients discovered 50% had Mg+ allergy. Eleven patients (20.75%) had the dystrophy in the family.
Table 6: Mean keratomertic values of astigmatism for different age groups
|
Age |
Sink |
Flat sink |
Steep sink |
CCT (µm) |
|
11-20 |
49.76 |
47.53 |
63.42 |
409.42 |
|
21-30 |
55.455 |
42.25 |
68.76 |
249 |
|
31-40 |
54.075 |
51.40 |
57.16 |
503.2 |
DISCUSSION
In this retrospective study we focused on the binocular vision and refraction in the patients of anterior corneal dystrophies. The culprit for excessive vision loss was corneal opacity and keratoconus, each of which was reported in 56.06% cases in this study. Keratoconus is a bilateral non-inflammatory corneal swelling having an incidence of approximately 1 per 2,000 in the common population (Rabinowitz, 1988). Keratoconus and other non-inflammatory corneal thinning disordes such as keratoglobus, pellucid marginal degeneration and posterior keratoconus are characterized by progressive corneal thinning leading to its protrusion and ultimately scarring. All these symptoms result in impaired vision. Its diagnosis is done by refraction, keratometry and corneal topographic analysis. Keratoconus is associated with irregular corneal astigmatism of inferior corneal steepening (Krachmer, 1984). The prevalence of keratoconus has been estimated in various studies to be as high as 2.2 per 1,000, 1 to as low as 4 per 100,000. The earliest changes observed in the histological structure of keratoconus are the presence of fibrillations, irregularities, and disruptions in Bowman’s layer. Activated stromal keratocytes and corneal epithelial cells may penetrate into the disrupted Bowman’s layer (de Toledo, 2003).
Uncorrected Refractive Error (URE) is a leading cause of visual impairment in urban China where over 70% of 15-year-olds have myopia which is quite similar to our results as we estimated the prevalence of myopia to be 77.78% in teenagers. Whereas in adults in sub-Saharan Africa, the prevalence of myopia and other refractive errors is far less (Sherwin and Mackey, 2013).
URE represents the most common cause of visual impairment worldwide and the second leading cause of blindness. Myopia is the most common refractive error globally, and it is estimated that there are 1.44 billion people affected, equal to 22.6% of the world’s population (Resnikoff et al., 2002). Myopia was reported in 33.96% of our subjects. Most probably it was caused due to keratoconus as it leads to the thinning of cornea. Chang et al. (2001) studied that changes in the anterior segments as the eyeball elongates in myopia progression included flatter corneal curvature, decreased corneal thickness and decreased endothelial density (Chang et al., 2001).
Hyperopia can affect both children and adults. Hyperopia may be passed from parents to the offspring. It affects about 5 to 10 percent of Americans. Ip et al. (2008) concluded that moderate hyperopia was strongly associated with many common eye conditions especially in older children (Ip et al., 2008). According to 2010 U.S. Age-Specific Prevalence Rates for Hyperopia by Age, and Race/Ethnicity, hyperopia was present in 6.42% Hispanics, 5.17% black Americans and 11.38% in white Americans while we estimated a prevalence of 15.09% in the Punjabi population. In US population, hyperopia is more prevalent among females (11.31%) than males (8.42%) whereas in our study we found more males (7.54%) to be affected than females (3.77%) (www.nei.nih.gov/eyedata/hyperopia.asp).
Corneal astigmatism is an imperfection in the curvature of the cornea. Lenticular astigmatism arises due to distortion in the shape of the lens. As a result of either type of astigmatism the vision becomes blurry. People may be born with astigmatism and they may also have other refractive errors (Lens et al., 2008). Pokharel et al. (2010) performed a retrospective study on the school going children of the urban and rural areas of Nepal and estimated a prevalence of 1.8% for astigmatism (Pokharel et al., 2010). In our study no case of astigmatism was noted in the age group of < 10 years where as astigmatism greatly affected the teenagers (80.0%).
Normal corneal thickness is about 540µm. We estimated a mean CCT of 409.2µm in the age group of 11-20 years, 249µm in the age group of 21-30 years and 503.2µm in the age group of 31-40 years. According to Cho P. and Lam C. the maximum decrease in central corneal thickness occurred in subjects in the age group of 10-25 years. Central corneal thickness decreased with increasing age (Cho and Lam, 1999).
From these observations it is concluded that most CDs exhibit variable phenotypes. Some may exhibit a clear cornea while some may have a cloudy cornea, affecting visual acuity to different levels. Corneal Dystrophies are suspected when corneal transparency is altered and corneal opacities occur spontaneously in both corneas, and especially in the presence of a positive family history or in the offspring of consanguineous parents. ACDs were found to predominate in males. Dystrophies were more prevalent in the age group of 11-20 years. Changes in the corneal thickness lead to refractive errors. Untreated cornea will proceed to vision loss. Some are treated medically or by excision of the defected corneal tissue, such as Penetrating Keratoplasty (PKP) and Phototherapeutic Keratectomy (PTK). Other less severe dystrophies do not require treatment. If left untreated, it leads to corneal blindness.
ACKNOWLEDGEMENTS
We sincerely thank the staff of General hospital and Layton Rehmatullah Benevolent Trust (LRBT) for their help in the clinical evaluation and data collection.
References