Journal of Infection and Molecular Biology
Short Communication
Prevalence of Brucellosis among Camels in District Muzaffargarh, Pakistan
Sami Ullah1*, Tariq Jamil2, Muhammad Hassan Mushtaq1, Muhammad Hassan Saleem3
1Department of Epidemiology and Public Health; 2University Diagnostic Laboratory; 3Department of Clinical Medicine and Surgery, University of Veterinary and Animal Sciences, Outfall Road (54600), Lahore, Pakistan.
Abstract | Brucellosis is an important zoonotic disease of animals and humans. Camel has often been neglected for brucellosis study in Pakistan due to many reasons. A study was conducted to investigate prevalence among camels in district Muzaffargarh. A total of 387 serum samples (300 females; 87 males) were collected and subjected to Rose Bengal plate test (RBPT) and polymerase chain reaction (PCR). Out of 387 samples, 2 (0.51%) were found seropositive by RBPT however, none of them was found positive by PCR. All the seropositive samples came from adult female camels (≥6 years of age) only. Common watering points (e.g. ponds) showed significant association (P<0.05), however, age and sex had non-significant association (P>0.05). The study concluded seroconversion and potential risk factor involved in the spread of brucellosis in camel herds. Routine screening together with public awareness is required to control brucellosis in the area.
Keywords | Seroprevalence, PCR, Brucellosis, Camels, Muzaffargarh
Editor | Tahir Yaqub, University of Veterinary and Animal Sciences, Lahore, Pakistan.
Received | May 16, 2015; Revised | May 18, 2015; Accepted | May 18, 2015; Published | June 03, 2015
*Correspondence | Sami Ullah, University of Veterinary and Animal Sciences, Outfall road, Lahore, Pakistan; Email: drsami888@gmail.com
Citation | Ullah S, Jamil T, Mushtaq MH, Saleem MH (2015). Prevalence of brucellosis among camels in district muzaffargarh pakistan. J. Inf. Mol. Biol. 3(2): 52-56.
DOI | http://dx.doi.org/10.14737/journal.jimb/2015/3.2.52.56
ISSN (Online) | 2307-5465; ISSN (Print) | 2307-5716
Copyright © 2015 Ullah et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Brucellosis is an important zoonotic disease of domestic and wild animals including humans (Hamdy and Amin, 2002; Radostits et al., 2007). Causative agents of Brucellosis are gram negative bacteria, belonging to genus Brucella, five out of nine known species have potential zoonotic significance (Godfroid et al., 2005; Seleem et al., 2010). Camel is known to be susceptible for both B. abortus and B. malitensis, but it is not considered as a primary host (Gwida et al., 2011; Wernery and Kaaden, 2002). Epidemiological reviews on camel brucellosis have shown a cosmopolitan prevalence (Abbas and Agab, 2002; Gwida et al., 2012; Seleem et al., 2010; Sprague et al., 2012). Camels get subsequent infection from other animals sharing their habitat and husbandry practices (Abbas et al., 1992). Clinical manifestation of this disease is in the form of reproductive loss leading to abortion, still birth or infertility (Olsen and Tatum, 2010). Camel plays important socio-economic role among nomadic pastorals of arid and semi-arid lands in the country (Ahmad et al., 2010). The pastoral households are at great public risk due to their close physical contact and assistance in calf delivery, cleaning new-borns, suckling and carrying the young calf from field to nomadic house (Abbas and Agab, 2002). Ingestion of unpasteurized milk and its products is a source of brucellosis transmission in humans (Shimol et al., 2012; Warsame et al., 2012). The disease could pose serious socio-economic threats to livestock owners in pastoral and rural community (Megersa et al., 2011). Previous studies have indicated brucellosis as endemic in livestock farms of Pakistan with increasing prevalence rates (Munir et al., 2011).
Despite its demographic and socioeconomic importance, data regarding camel brucellosis remains scanty and restricted to other food animals in the country (Abubakar et al., 2012; Gul and Khan, 2007). For accurate diagnosis serological tests like Rose Bengal plate agglutination test (RBPT) are cheap and easy for herd based screening of animals with high sensitivity and low specificity (Ali et al., 2013; Ghanem et al., 2009; OIE, 2012). Confirmation of seropositive animals by more specific antigen based tests, like indirect-ELISA and PCR are helpful in interpreting diagnosis more accurately (Gall and Nielsen, 2004; Schelling et al., 2003).
Muzaffargarh is located between 30.0703° N-71.1933° E in south-west of Punjab province, at the bank of river Chenab of Pakistan. The district comprises of four administrative divisions i.e. Kot Addu, Muzaffargarh, Jatoi and Alipur. The area is rich in camel and cattle population having arid ecology with 102110 acres of forested area. This district was severely affected by Indus and Chenab river floods in 2010 (Figure 1). The present study estimated the prevalence and associated factors of brucellosis among camels of district Muzaffargarh by Rose Bengal plate agglutination test (RBPT) and polymerase chain reaction (PCR) for seroprevalence and molecular diagnosis respectively. This was the first time to study camel brucellosis through molecular identification in the district.
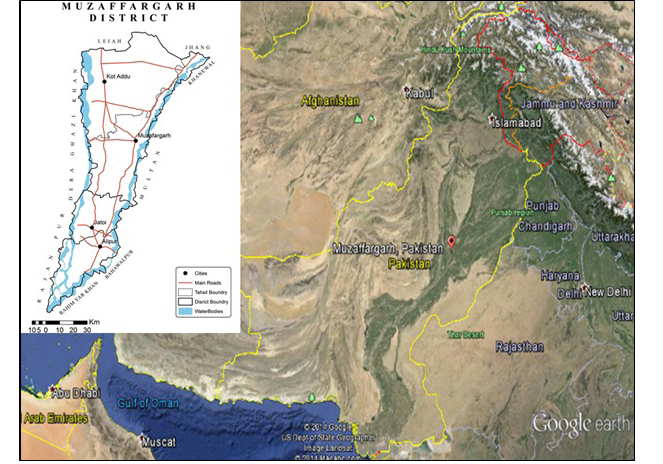
Figure 1: Location map of district Muzaffargarh
A total of 387 blood samples were collected randomly from different camel herds (> 6 months of age) among four divisions of district Muzaffargarh along with various study factors. These samples were initially screened by RBPT. Serologically positive samples were then processed for genome extraction and PCR. Sample size was determined by assuming population unknown, prevalence 50% and confidence interval 95% in the formula (Thrusfield, 2007).
Serum drawn from blood samples were initially screened for RBPT as described previously (Alton et al., 1975). Standardized antigens were collected from Biologicals Supply Section, Veterinary Research Institute, Zarar Shaheed Road, Lahore (54810).
Brucella genome was extracted and purified by using QIAmp DNA Mini Kit (Qiagen, Germany) according to manufacturer’s instructions. Genome quantity and quality was measured by NanoDrop 2000 UV-Vis Spectrophotometer (Thermo Scientific, USA). The extracted genome was amplified for polymerase chain reaction by using brucella genus specific 223 primers targeting outer membrane protein encoding gene (bcsp 31). Polymerase chain reaction technique was used for molecular identification of brucellosis in the samples. PCR was performed in 25 μL reaction mixture as described previously (Gemechu et al., 2011) having concentrations of 20 pmol of primers (Table 1), 0.2 mM dNTPs (10mM), 1× PCR buffer, 1.5 mM MgCl2, 0.5 U Taq DNA polymerase, and 10 μl of template DNA. Cycle conditions consisted of initial denaturation for 5 min at 93°C, template denaturation at 90°C for 1 min, 30 sec of primer annealing at 58°C and final extension at 72°C for 7 min 40 cycles.
Table 1: Primers used for PCR targeting BCSP31 gene
|
Type of Primer |
Primer sequence |
Product size |
|
Forward Primer |
5-TGGCTCGGTTGCCAATATCAA-3' |
223 bp |
|
Reverse Primer |
5-CGCGCTTGCCTTTCAGGTCTG-3' |
Table 2: Association between seroprevalence of brucellosis in camel herds and studied parameters using Chi-square analysis
|
Parameters |
Seropositive |
Seronegative |
P-value |
|
|
Age |
≤ 6 years >6 years |
00 2 |
87 298 |
0.445 |
|
Sex |
Male Female |
00 2 |
133 252 |
0.305 |
|
Herd composition |
Only camels Mixed herd (other animals) |
2 00 |
355 30 |
0.681 |
|
Water Source |
Rivers Ponds Traditional wells |
00 2 00 |
87 93 205 |
0.046 |
PCR products were visualized on 1.5% agarose gel stained with ethidium bromide (10 mg/ml) under UV-light using gel documentation system (Bio-Rad, USA).
Pearson’s Chi-square analysis was used to determine association of the factors with the positivity of the infection with 95% confidence interval.
Out of 387 camel blood samples, 2 (0.51%) camels were found positive by RBPT. Followed by PCR and Gel Electrophoresis, the samples were found negative. Out of 387 camel serum samples, 300 (77.51%) samples came from adult (≥6 years) animals whereas, remaining 87 (22.49%) samples came from younger (<6 years) animals. The two seropositive samples had come from adult animals whereas younger animals were found all negative by RBPT. Based upon sex of animals, 133 (34.4%) of the total samples came from male camels whereas 254 (65.63%) came from female camels. The two seropositive samples were found both form female camels (0.78% prevalence rate among female camels). Among risk factors studied, watering points showed a significant association for brucellosis transmission (P<0.05) (Table 2).
A total of 387 camel blood samples were processed by RBPT by which two samples were found positive showing overall 0.51% seroprevalence. Previous studies in Pakistan have reported 0.0-17.2% seroprevalence among camels (Ahmad and Munir, 1995; Ajmal et al., 1989; Gul and Khan, 2007; Gul et al., 2014; Nasrin et al., 1998). Higher seroprevalence of brucellosis among livestock of intensive/semi-intensive system may be indicative of transmission through close contact (Abbas and Agab, 2002). Historical isolation and nomadic raising system may have prevented camel herds from brucellosis in the area. Although brucellosis is less prevalent in camels than cattle and buffaloes, consuming raw camel milk may threat human health for infection transmission. Other studies have revealed a seroprevalence ranging between 0.3-3.9% in different areas of Africa (Ghanem et al., 2009; Megersa, 2004; Omer et al., 2000). Herd composition, especially mixing of small ruminants (sheep and goats) is known for prevalence of brucellosis in camels (Abbas and Agab, 2002; Omer et al., 2000). The camel herds, in the present study, were not mixed with other livestock species neither had prior vaccination history. However, lack of vaccination against brucellosis may be reason for the existing infection among herds. Vaccination can be suggested for minimizing the infection level among camel herds, however the control remains questionable (Dawood, 2008; Treanor et al., 2010).
Molecular identification of seropositive samples by PCR revealed 0 (0%) detection for brucellosis. Higher seroprevalence by RBPT reveals its high sensitivity but low specificity. This may be true due to fluctuating antibody titers and/or presence of antibodies in healthy animals where disease is endemic (Gul and Khan, 2007; Gwida et al., 2011). RBPT antigen is also reported to cross-react with Salmonella urbana, Yersinia enterocolitica and E. coli that further questions its specificity (Abubakar et al., 2012; Gall and Nielsen, 2004). PCR is more reliable than serological tests but its efficacy remains highly variable (Khamesipour et al., 2014; Hassanain et al., 2012).
Seroprevalence of brucellosis was found higher in females 2/254 (0.87%) than males 0/133 (0%). Similar results were found in a study at Karachi where females and males were found 1.8% and 0% seroprevalent respectively (Siddiqui, 2009). Our results were also supported by (Abbas and Agab, 2002; Bekele, 2004; Omer et al., 2010; Teshome et al., 2003; Warsame et al., 2012), however contradicted by (Gul et al., 2014; Tassew and Kassahun, 2014) who found slightly higher prevalence rate in male camels. This higher prevalence have been attributed to pregnancy, lactation, physiological differences of females than males and the presence of erythritol (Gyles et al., 2008; Radostits et al., 2007; Warsame et al., 2012). However, the association of sex with the seroprevalence of brucellosis was found insignificant (P>0.05).
Regarding age, adult animals were found more seroprevalent i.e. 0.7% (≥ 6 years) as compared to 0% (≤ 6years). Adult camels have also shown higher seroprevalence rates elsewhere (Abbas and Agab, 2002; Omer et al., 2010). Age, in our study, didn’t show significant association with the seroprevalence of brucellosis (P>0.05) as supported by (Amin et al., 2005; Ghanem et al., 2009; Teshome et al., 2003; Tilahun et al., 2013).
Watering sources, in the study area, were composed of some fixed points like ponds and traditional wells shared by humans and all kind of livestock prevailing in that area. These watering sources showed statistically significant (P<0.05) association with the seropositivity of the infection. This seropositivity cloud have been associated in a variety of ways e.g. (i) drinking of contaminated water by discharges of infected animals (ii) physical contact with sub-clinical infected animals while taking rest at these common places.
The study can conclude that, among camels, both sexes are susceptible for brucellosis irrespective of age. Herds mixed with other animals and sharing common watering points may show higher prevalence rates than isolated and independent water source herds.
Public awareness is needed as preventive regimen especially in nomads. Routine screening and culling of seropositive animals is recommended among herds at least on annual basis. Vaccination of animals can be recommended in disease endemic areas, provided that its cost-effectiveness and profitability studied earlier (Roth et al., 2003). For human prevention, public awareness is recommended not to consume raw/unpasteurized milk. In the study it was found that 94% of the herd owners consumed raw milk, 4% boiled and 2% sour milk. Further studies may include population based prevalence study, antigen based identification of the etiology through ELISA/PCR and calculation of Odd’s ratio for associated rick factors among camel herds of Punjab.
Acknowledgments
Author is thankful to department of Epidemiology and Public Health, University of Veterinary and Animal Sciences, Outfall road, Lahore for conduction of study. Author is also thankful to Prof. Dr. Masood Rabbani, Dr. Fariha Akhtar and Javed Muhammad for their cooperation at University Diagnostic Laboratory.
Conflict of Interest
The authors declare no conflict of interest to disclose.
References





